A recent Senate Judiciary Committee report has accused UnitedHealth Group (UHG), the largest provider of Medicare Advantage (MA) plans, of using aggressive tactics to boost payments from the federal government. Released on January 12, 2026, by Sen. Chuck Grassley (R-Iowa), who chairs the committee, the 105-page document is titled “How UnitedHealth Group Puts the Risk in Medicare Advantage Risk Adjustment.” It claims the company has turned risk adjustment—a key part of how MA plans are paid—into a major profit-making operation, going against the program’s original purpose.
What Is Medicare Advantage and Risk Adjustment?
Medicare Advantage, also known as Medicare Part C, lets private insurers like UnitedHealth manage health benefits for seniors and some disabled people instead of traditional Medicare. The government pays these insurers a fixed monthly amount per enrollee. This payment is adjusted based on the enrollee’s health: sicker patients with more documented conditions receive higher payments to cover expected higher costs. This process is called risk adjustment.
The system aims to make sure insurers are fairly compensated for covering people with serious health issues. However, critics argue it can be abused if companies add or emphasize diagnoses that may not fully reflect actual treatment needs, leading to higher payments without necessarily improving care.
Key Findings from the Senate Report
The report is based on more than 50,000 pages of internal UnitedHealth documents, including training materials, policies, software details, and audit tools, which the company provided in response to Grassley’s requests.
Investigators found that UnitedHealth captures more diagnoses and diagnosis codes than other MA organizations. This results in higher risk scores and larger payments from the Centers for Medicare & Medicaid Services (CMS) compared to competitors. The report describes these as “aggressive strategies” to maximize scores.
Examples include:
- Sending nurse practitioners on home visits (through the HouseCalls program) to assess patients’ health and document conditions.
- Using AI, data analysis, and point-of-care testing to identify potential diagnoses.
- Adding codes based on probabilities, related conditions, or loose criteria rather than strict evidence.
The report notes that many diagnoses lack clear, universal definitions, making it hard to judge if they are appropriate. It highlights a case with dementia codes: CMS removed them from risk adjustment in 2014 due to upcoding concerns, then re-added them in 2020. After that, dementia diagnosis rates in MA plans rose 11.5% compared to traditional Medicare.
Because UnitedHealth is so large and integrated (with its own data tools and services sold to other insurers), its practices can spread quickly across the industry. The report says this gives bigger companies an edge over smaller ones and helps them stay ahead of CMS efforts to curb excessive coding.
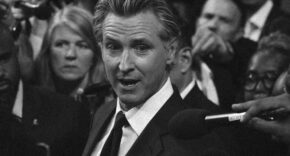
Grassley, who helped create the MA program as Senate Finance Committee chair in 2003, called for stronger oversight. He said bloated spending harms taxpayers and the program. “My investigation has shown UnitedHealth Group appears to be gaming the system and abusing the risk adjustment process to turn a steep profit,” he stated. “Taxpayers and patients deserve accurate, clear-cut and fair risk adjustment processes.”
UnitedHealth’s Response
UnitedHealth strongly disagreed with the report’s claims. In statements to media outlets, the company said its coding practices and HouseCalls program follow CMS rules. It pointed to government audits showing ongoing compliance, plus strict quality controls and safeguards.
“We regularly engage with CMS, the committee and others on ways to improve programs that keep seniors healthier and more independent,” a spokesperson said. The company emphasized its focus on lower costs, better access, and higher-quality care for MA enrollees. It also released its own reports highlighting the value of Medicare Advantage to the government and beneficiaries.
Broader Context
The investigation began in February 2025 after articles in The Wall Street Journal and other outlets raised questions about UnitedHealth’s billing. It builds on earlier reports of upcoding and a federal probe by the U.S. Department of Justice into MA practices, which UnitedHealth acknowledged in 2025.
As MA grows—now covering more than half of Medicare beneficiaries—the program spends billions in taxpayer dollars. Grassley stressed Congress’s duty to oversee it closely to prevent misuse.
This report adds to ongoing debates about whether risk adjustment encourages better care for sick patients or allows insurers to inflate profits. While no formal wrongdoing was proven in the document, it calls for fairer processes to protect both seniors and public funds.